Tuberculosis (TB) is a serious bacterial infection which is spread through inhaling tiny droplets from the coughs or sneezes of an infected person. TB mainly affects the lungs, and is treated with antibiotics. Each year, World Tuberculosis Day falls on 24 March, the date in 1882 when Dr Robert Koch announced that he had discovered the bacterium that causes tuberculosis.
Technology has dramatically moved forward since the early identification of the bacterium by Dr Koch over 130 years ago. Assistant Professor Rick Ong‘s research group is working on a project to identify and catalogue the whole genome sequences of over 1,000 different strains of TB within countries in Southeast Asia. Whole genome sequencing identifies the complete DNA sequence of an organism’s genome at a single time — in this case, the strains of the TB bacterium.
Looking back on the work you’ve undertaken, which project stands out as memorable?
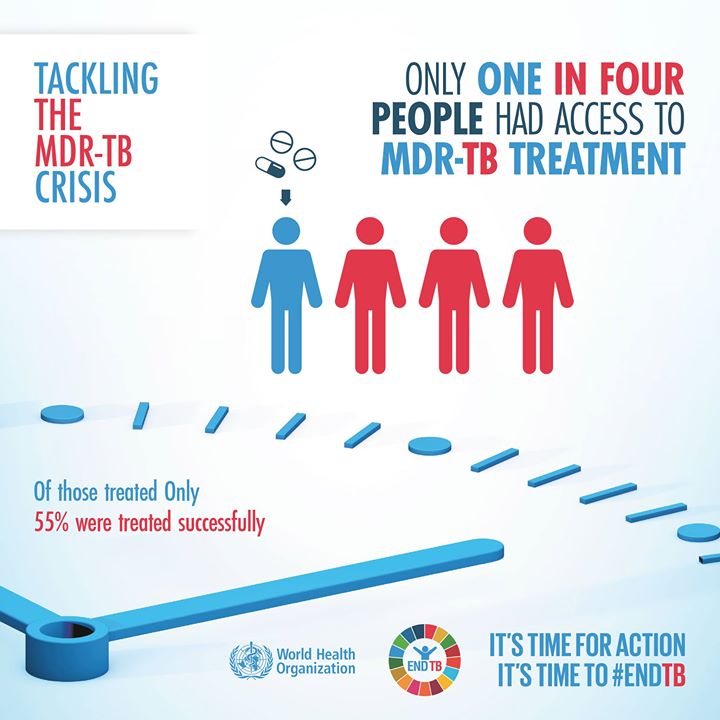
Rates of TB in Singapore have declined from more than 300 per 100,000 persons in the 1960s to 38.4 per 100,000 persons in 2015. Despite this, we are seeing an emergence of drug-resistant tuberculosis, such as multidrug-resistant tuberculosis (MDR-TB), that are resistant to two of the most effective antibiotics against TB. Treatment of drug-resistant TB would require the use of second line drugs that are costlier and generally result in more side effects in patients.
MDR-TB is emerging due to multiple reasons such as overuse of antibiotics and patients not finishing the full antibiotic course. This poses a serious threat to public health worldwide as TB is getting harder to treat.
One of my most memorable pieces of work is the use of whole genome sequencing to identify groups of people or ‘clusters’ with MDR-TB in Singapore. We worked with public health teams to confirm or dispute clusters, using information acquired to understand how the infection is spread, what treatment to give, and what measures are needed to prevent further spread of the infection.

One of my most memorable pieces of work is the use of whole genome sequencing to identify groups of people or ‘clusters’ with MDR-TB in Singapore. We worked with public health teams to confirm or dispute clusters, using information acquired to understand how the infection is spread, what treatment to give, and what measures are needed to prevent further spread of the infection.
One MDR-TB cluster was a group of young male Singaporeans who spent considerable time in a gaming cafe. Whole genome sequencing identified that they were all infected with the same TB strain that was nearly identical to that of another individual diagnosed 4 years earlier. Further investigations uncovered that one of the infected males from the gaming cafe was an ex-colleague with the earlier diagnosed individual, even though they did not know each other. This case illustrates how easily infectious diseases such as tuberculosis can spread in Singapore, and it highlights the challenges in identifying TB contacts since this is a disease that can manifest only years later.
What are you currently working on?
We are currently working on an international project to catalogue the whole genome sequence of different TB strains globally. The catalogue is a huge resource; for example, it can be used to identify treatments that are more effective against drug-resistant strains, as well as distinguish genetic markers of antibiotic resistance to identify emerging clusters of drug resistance early, so that measures can be put in place to prevent the spread.
Our group is hoping to include TB strains from across the Southeast Asian region that are causing outbreaks. This will help us to monitor their spread and hopefully prevent local epidemics through greater understanding of these strains.
What’s been the biggest change you’ve seen in your research area?
I would have to say it’s the development and use of molecular techniques to identify TB drug resistance for effective treatment of individual patients. Previously, it would have taken months to determine which antibiotics would be effective and should be administered. Now, this can now be done in a single test that would only take about a week.
UK is the first to use TB whole genome sequencing as a diagnostic test. Patients can be treated with the right medication more quickly, thus slowing the spread of the disease and reducing the risks of increased drug resistance.
If you could make one change to positively impact public health what would it be?
Although this approach of rapid whole genome sequencing is a benefit, there is a risk that genomics could be misused and thus should not be the sole intervention in tackling drug-resistant tuberculosis. We should work to identify the root causes of drug-resistant tuberculosis (as well as other bacterial infections) and act to prevent further emergence of drug-resistant strains. There is also the need to examine the factors resulting in over-prescription of antibiotics and understanding why patients don’t finish the whole course of antibiotics.
Infectious diseases respect no borders — people get on planes and spread infections. There is an increasing understanding that countries need to work together to monitor and respond to emerging infections including the spread and increase of antimicrobial resistance.
There are real opportunities in establishing timely information sharing, although barriers remain around data privacy, security concerns and a lack of consistent and comprehensive data in some countries.
I am optimistic that having a global TB molecular surveillance database will lead to better treatment and control of tuberculosis, in particular drug-resistant tuberculosis.
Tell us something surprising about you that people may not know.
I have a TV but it is not connected. Our television at home is purely decorative. We disconnected it over a year ago and we haven’t missed it since!