Collaborative Solutions Targeting Antimicrobial Resistance Threats in the Health System (CoSTAR-HS)
Collaborative Solutions Targeting Antimicrobial Resistance Threats in Health Systems (CoSTAR-HS)
Antimicrobial resistance (AMR) is a major global public health threat. At the 71st meeting of the United Nations General Assembly in September 2016, world leaders pledged to work at national and international levels to address the rising threat of AMR. AMR rates are high in Asia – including Singapore – relative to many parts of the world, and it is one of the key infectious diseases issues identified as major research focus areas for Singapore’s Research, Innovation and Enterprise plan.
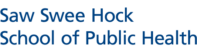
CoSTAR-HS was funded to build up capacity, infrastructure, and networking opportunities for AMR research in Singapore under the National Medical Research Council’s (NMRC’s) Centre Grant call in October 2016. The funding was renewed in December 2021 to build on and enhance the prior strategy that has fundamentally remained unchanged since its inception in 2017. It is a partnership involving researchers and clinicians from the National University Health System (NUHS), Singapore General Hospital (SGH), and the National Centre for Infectious Diseases (NCID). The new partner institution for the CoSTAR-HS renewal is the National University Polyclinics (NUP) – a key partner for crucial research on AMR in primary care.

Research Strategy
Our research strategy is to perform clinical- and policy-relevant AMR research, while consequently strengthening institutional and national AMR research capacity through a collaborative approach.
Our focused research areas are:
- Expansion of CoSTAR-HS to address the critical issues of AMR in primary care systematically.
- Improve the management of severe drug-resistant infections (DRI’s) – clinical trials and precision medicine focus.
- Improve infection prevention in healthcare institutions – focus on carbapenemase-producing Enterobacterales (CPE) and environmental microbiomes
- Facilitate science-based policies addressing AMR at an institutional and national level.
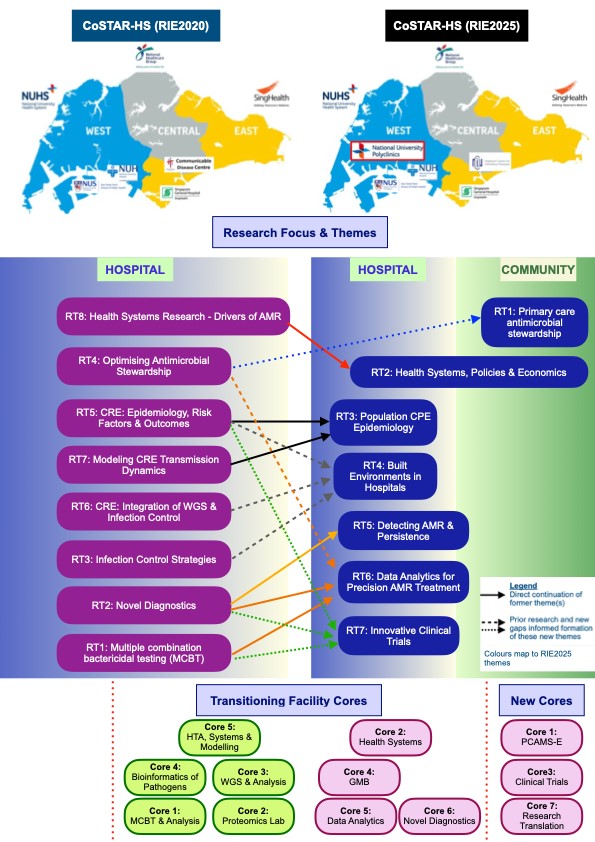
Facility Cores
Click here for more details on each Cores
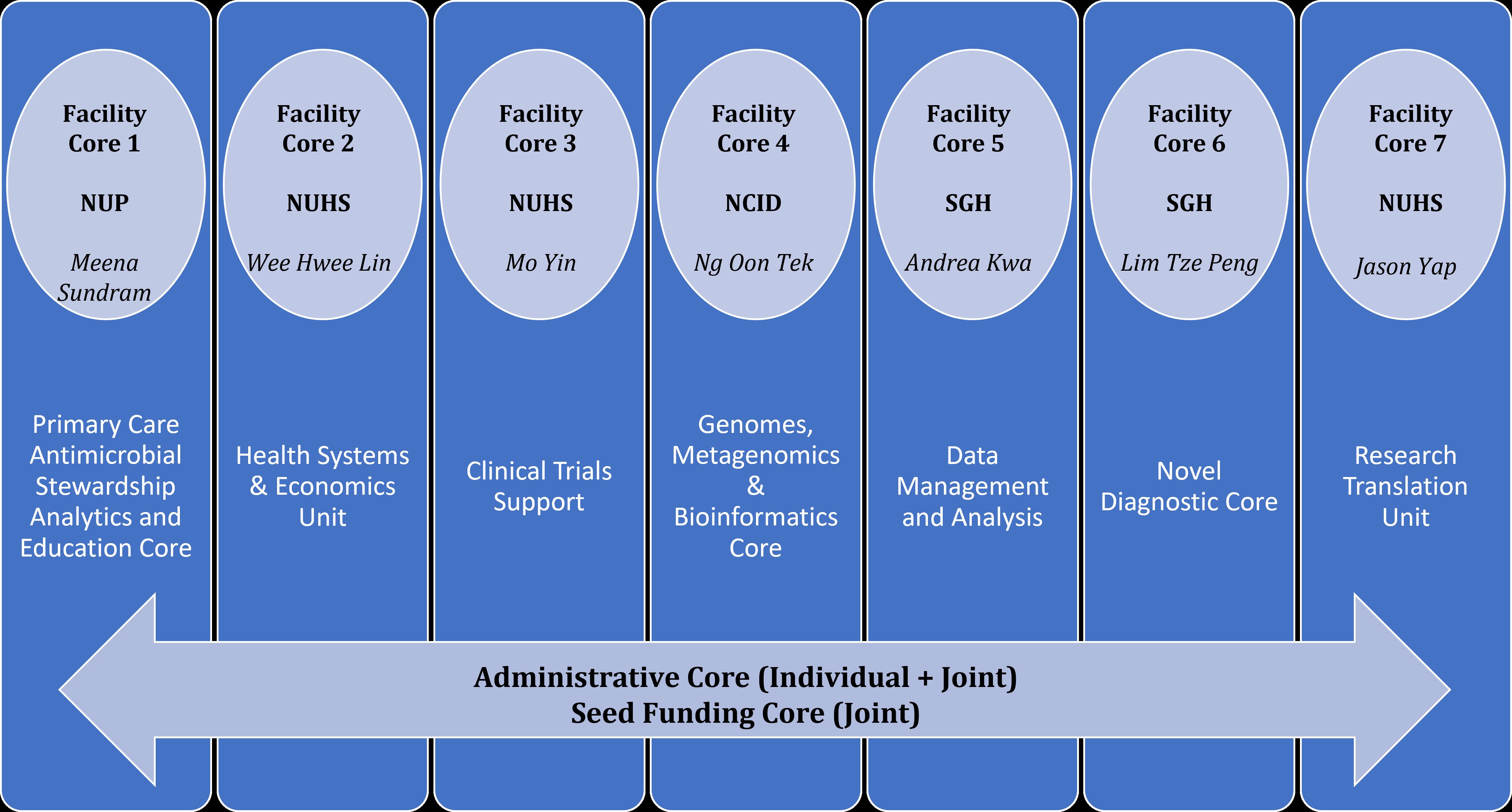
Facility Core 1: Primary Care Antimicrobial Stewardship Analytics and Education Core
Hosted at NUP, this facility aims to meet this collaborative proposal’s primary care antimicrobial stewardship analysis and intervention needs. We anticipate collecting and analyzing 4,000 urine culture samples and 2,500 wound swab culture samples to support the routine antibiogram and surveillance proposed in the various themes in this proposal. Crucial to the Core’s purpose of continuing to deliver timely, clinically important data of this Facility Core aims to expand the Core’s analysis capacity by acquiring additional equipment, such as laptops and statistics software. The Facility core will provide funding for educational interventions and IT systems configuration and maintenance for data analysis.
Contact person: Dr Meena Sundram
Email: Meena_SUNDRAM@nuhs.edu.sg
Facility Core 2: Heath Systems & Economics Unit
Hosted at NUHS, the purpose is to retain and build the manpower capacity and expertise on economics, health systems, and mathematical modeling research relevant to AMR. Other functions include maintaining access to specialized software and other equipment necessary for such research and facilitating access to cross-institutional clinical and health economics data relevant to AMR research.
Contact person: Dr Wee Hwee Lin
Email: weehweelin@nus.edu.sg
Facility Core 3: Clinical Trials Support
Hosted at NUHS, this facility aims to support local sites for both international and local clinical AMR trials.
Contact person: Dr Mo Yin
Email: mdcmy@nus.edu.sg
Facility Core 4: Genomes, Metagenomics & Bioinformatics Facility Core
Hosted at NCID, this facility aims to meet this collaborative proposal’s whole-genome and metagenomic sequencing and analysis needs. We anticipate that the current collaborative group will require dedicated sequencing capability. In the initial iteration of CoSTAR-HS, demand for sequencing exceeded our projected amount, although we could eventually support this work via funding from competitive grants. We anticipate that we will sequence and analyze at least 4,500 samples to support the translational work proposed in the various themes in this proposal. Crucial to the Core’s purpose of delivering timely and clinically important data, the facility aims to expand the Core’s sequencing and analysis capacity by acquiring additional equipment. Please use attached form for the use of the facility.
Contact person: A/Prof Ng Oon Tek
Email: oon_tek_ng@ncid.sg
Facility Core 5: Data Management and Analysis
Hosted at SGH, the purpose of this facility core is to build appropriate infrastructures and platforms in Computational Biology and Artificial Intelligence for data accessing, storage, sharing and analysis of omics data together with electronic health records in real-time to enable public health and clinical management, clinicians, and researchers to easily access the data and derive meaningful information to improve medicine, healthcare services and performance. Moreover, it enables data interoperability and sharing easy and secure across different institutions.
Contact person: A/Prof Andrea Kwa
Email: andrea.kwa.l.h@sgh.com.sg
Facility Core 6: Novel Diagnostic Core
Hosted at SGH, this facility aims to provide bacteria omics and flow cytometry expertise to meet the needs of this collaborative platform. These include:
- Resistance determinant discovery
- Untargeted bacteria proteomics
- Quantitative bacteria proteomics
- High-throughput screening for antimicrobial susceptibility
- Single-cell assessment of bacteria responses to antimicrobials
Contact person: Dr Lim Tze Peng
Email: lim.tze.peng@sgh.com.sg
Facility Core 7: Research Translation Unit
Hosted at NUHS, the purpose of this facility core is to improve the translational research environment, specifically for AMR. It will work with research teams within CoSTAR-HS to connect their work with policymakers, healthcare institutions and industry. It will specifically facilitate the achievement of several proposed translational outcomes and indicators of CoSTAR-HS.
The key functions are:
- Dissemination of research findings.
- Working with stakeholders to implement research findings as relevant evidence-based policies and/or clinical practice.
Contact person: Dr Yap Chin Huat Jason
Email: jasonyap@nus.edu.sg
Research Themes and Aims
There are 7 research themes within CoSTAR-HS:
- Primary Care Antimicrobial Stewardship (PC-AMS) – Optimizing antibiotic prescribing in primary care
- To study the prevalence of antibiotic-resistant bacteria causing common infections (such as UTIs and soft tissue infections (STIs)) that are managed in the primary care setting, establishing routine surveillance and isolate collection for these bacteria for subsequent analysis. These data and isolates will generate new research hypotheses and pave the way for further collaborations with partner institutions. After cross-validation with data from other primary public healthcare institutions and international antimicrobial guidelines, these data can also be used to develop relevant and time-sensitive local guidelines.
- To program a new in-built function within our IT systems to collect and analyse data on the prevalence of infections, indications, and appropriateness of antibiotic prescriptions, as well as the prescribing habits of primary care physicians. These data will be used to understand physicians’ knowledge, attitudes, practices, perceptions, and barriers that will inform subsequent interventions to optimise antimicrobial stewardship.
- To develop educational and clinical interventions to strengthen the rational prescription of antibiotics in primary care. Outcomes of interventions will be assessed. Interventions implemented at NUP may then be similarly and subsequently implemented in private general practices and other primary public healthcare institutions.
- Health systems, policies, and economics in AMR control
- To identify and evaluate policies, programmes and structures that address AMR both locally and, in the region, using an adapted governance framework.
- To examine the motivations, social constructs, contextual drivers, and power relations of policy actors that influence behaviours and decision-making processes in developing policies for AMR, specifically in relation to the AMR control in primary care and hospitals.
- To assess the health systems barriers comprehensively and facilitators (including but not limited to surveillance, stewardship and infection prevention and control) to address AMR in the community.
- To develop strategies and tools for working with policymakers to implement AMR control policies in human health effectively.
- Population CPE Epidemiology To Guide Infection Prevention
- To determine the ongoing sources of endemic XDR-GNB transmission following the intensification of CPE infection prevention measures: the next 5 years (2016 to 2020).
- To determine the impact of Covid-19 on XDR-GNB population transmission.
- Built environment: The Achilles heel of MDRO control in healthcare facilities
- To explore environmental microbiome and bacterial genomics to identify factors associated with persistence and onward transmission of MDROs.
- To improve existing infection prevention and control (IPC) strategies and explore novel technologies to prevent environment-mediated infections with MDROs.
- Detecting Antibiotic Resistance and Bacterial Persistence to Identify Innovative Treatment Strategies against XDR-GNB
- To employ a systems biology approach integrating multi-omics (genomics, transcriptomics and proteomics) data to construct network models to describe antibiotic resistance and bacterial persistence.
- To push the boundaries of pharmacokinetic/pharmacodynamic (PK/PD) translational research by improving our current in vitro combination testing platform to improve turnaround time and identify novel diagnostics and innovative treatment strategies.
- Benchtop-to-bedside and beyond: Incorporating analytics and augmented intelligence (AI) strategies for the treatment of infections caused by multi-drug resistant organisms (MDROs)
- To leverage on existing health information technology (IT) to build an XDR-GNB data lake that includes clinical and outcome data of patients infected by XDR-GNB, phenotypic and genomic data of the infecting XDR-GNB, as well as results of more extensive testing of the isolates (such as proteomics and MCBT data) where available. We currently have more than 6,000 inpatient datasets with their archived XDR-GNB in our registry, growing at approximately 1,200 per year in SGH.
- To develop prediction models and machine learning systems with our XDR-GNB data lake in the exploratory development of a patient-centric, individualised-management approach that delivers the “right drug at the right dose for the right patient at the right time” for both empiric and targeted therapies against respiratory tract infection including pneumonia, and urinary tract infection (which constituted the top 2 highest infectious diseases burden in Singapore).
- Innovative Clinical Trials
- To develop novel clinical trial methodologies to improve the efficiency of trial conduct, maximise data utility and accelerate evidence synthesis.
- To expand local capacity in trial development, implementation and support and establish regional and industrial partnerships to build rapid trial pipelines.